Is HRV (Heart Rate Variability) a crucial metric in assessing our overall health and fitness? In this article, we delve into the intricate details of HRV, its correlation with the autonomic nervous system, and how it mirrors the delicate equilibrium between our body’s parasympathetic and sympathetic activity.
Plus, we’ll take a look at all the different factors that can influence HRV, like our mood and training status, to give you some valuable insights on how to optimize your performance levels. Join us as we explore the intriguing concept of HRV and how it can greatly influence our well-being and athletic potential.
WHAT IS HEART RATE VARIABILITY?
Heart rate variability (HRV) is an important indicator of overall health and fitness as it reflects the balance between your body's parasympathetic (i.e., “rest and digest”) nervous system and sympathetic (i.e., “fight or flight”) nervous system.
WHAT DOES HRV MEASURE?

FACTORS THAT INFLUENCE HRV
The beat-to-beat changes in heart rate, otherwise known as HRV, are heavily influenced by various factors.
MOOD AND MOOD DISORDERS
OBESITY, HIGH BODY MASS INDEX (BMI), AND WEIGHT GAIN
EXERCISE
SLEEP
SUBSTANCE USE
STRESS
Stressful experiences and stress levels affect HRV. The more we feel stressed, the higher the chance we will have lower HRV values. Indeed, HRV can be part and parcel of indexing stress levels at the physiological level.
GENDER
Many athletes may try to use HRV as an index of “readiness” and “recovery”, while they are not necessarily wrong to do so, they need to consider the many factors that influence HRV.
For athletes who track their HRV and heart rate, we recommend they take into account their qualitative experience. Don’t let HRV data replace your intuition.
WHAT IS GOOD HEART RATE VARIABILITY?
IMPROVED COGNITIVE FUNCTIONING
BETTER EMOTIONAL REGULATION
WHAT IS BAD HEART RATE VARIABILITY?
Low HRV can result from stress, poor sleep, unhealthy lifestyle habits, and certain medical conditions.
HOW TO MEASURE HEART RATE VARIABILITY?
COMMON HEART RATE VARIABILITY MONITORS

HOW DO SMARTWATCHES AND RINGS MEASURE HRV?
HOW TO CALCULATE HRV?
Best practices suggest that we need to consider mean heart rate before assessing HRV because higher heart rates are associated with lower HRV. In other words, if every other variable stays the same, a higher mean heart rate will naturally have a lower HRV (e.g., 60 BPM will have a lower HRV than 45 BPM)32.
BEST HRV MEASUREMENT PRACTICES

As we have discussed, HRV is subject to immense variability due to a multitude of factors. With this in mind, it is crucial that you account for several factors each time you take an HRV measurement for accurate and reliable data. Many people are familiar with circadian rhythms, which are psychological and physiological biological changes that occur in the body in 24-hour intervals. As you might have guessed, HRV is subject to that circadian rhythm. For this reason, it is crucial to measure HRV at the same time every day5. For accurate HRV measurements, be sure to avoid ingesting caffeine beforehand.
Caffeine is known to affect HRV measurements. Sleep quality and quantity are heavily associated with HRV measurements, so try to get consistently good sleep23. The brain has a connection to the heart, which means your mood can alter HRV. Try to maintain a consistent mood for the most reliable results. At the very least, be mindful of your mood each day and consider that when measuring HRV.
Additionally, higher HRV can often result from consistent exercise. However, HRV is temporarily lower during and shortly after exercise23. It is best to exercise after taking an HRV measurement so results aren’t skewed. Posture and small movements affect the cardiovascular and autonomic nervous systems. When taking an HRV measurement, be as still as possible while maintaining the same posture23.
Each of the factors above can have an effect on some of the systems that contribute to an HRV measurement. Please note that this is not a limited list. If you choose to track your HRV, ensure consistency in your measurement process.
HOW TO IMPROVE HEART RATE VARIABILITY?
Lower HRV is consistently associated with stress.
Do your best to downregulate, or lower feelings of stress. Coping strategies that alleviate stress can vary for each person, but try to find what works best for you; e.g., a ski tour, a mellow climb, or a run can be very helpful. Sometimes, a nice walk or meditation is the right answer.
A sedentary lifestyle is associated with lower HRV, and while this is not a risk for athletes, overtraining is. Make sure to manage your training effectively, so you don’t overtrain. Remember, we get stronger when we recover, not when we train. Eat a well-balanced diet to help maintain a healthy body. Finally, avoid unhealthy habits such as smoking or excessive alcohol consumption. Review how much caffeine you’re drinking, many athletes love coffee, but too much can affect HRV.
NORMAL HEART VARIABILITY RANGE
Unfortunately, there is not a specific HRV score that would be considered healthy for everyone. It is challenging to interpret HRV measurements, and these scores are subject to variability, given the multitude of lifestyle and psychological factors. If you think your heart rate variability is low (or are concerned about your HRV values), you should see a physician.
However, there can be some range fluctuations in HRV scores regarding gender and age; see the chart below.
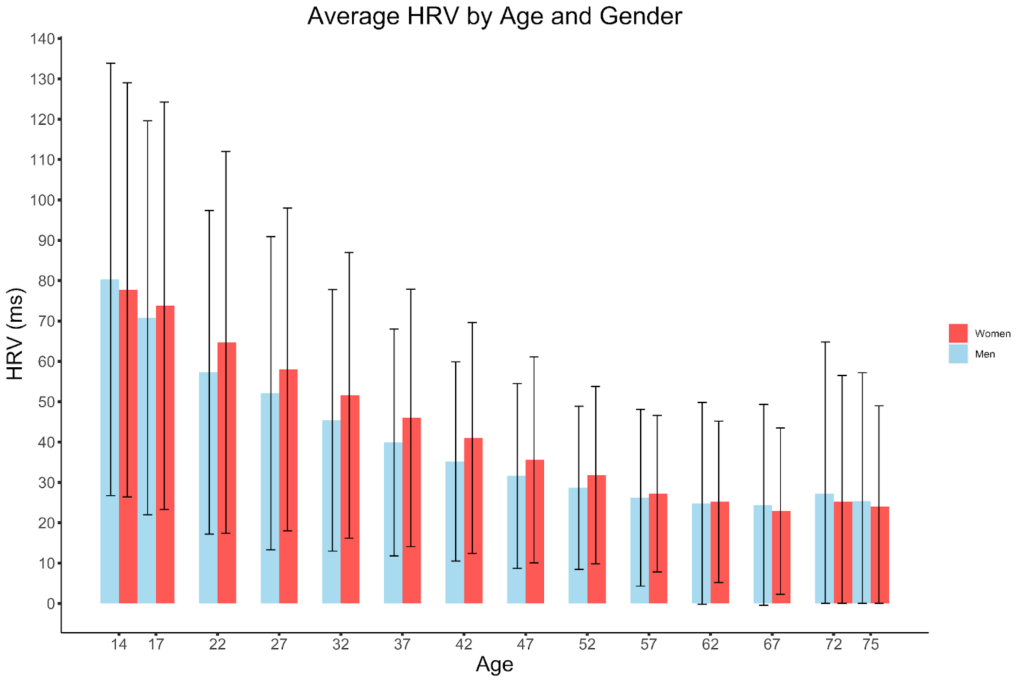
HEART RATE VARIABILITY BY GENDER
Prior to menopause, women generally have higher HRV compared to men. Research has found that estrogen helps increase the parasympathetic nervous system's influence on heart activity28.
HEART RATE VARIABILITY BY AGE
WHAT SHOULD YOU DO WITH HRV DATA?
If you choose to measure HRV on your own, make sure you follow a strict protocol (outlined above). This includes measuring HRV at the same time each day.
We don’t recommend using HRV to track your fatigue, recovery state, and fitness. Instead, we urge you to pay attention to other things affecting your training and overall health. For instance, be mindful of your sleep patterns, food, stress, and mental health. Are you sleeping enough? Is your sleep quality good? Are you regularly using caffeine and alcohol? How about other recreational substances? How are those affecting your sleep and training? Are you eating a balanced diet? Are you stressed at work? At home? Do you have stress management tools that you can use? Are you feeling recovered after recovery workouts? Do you have a regular workout that you can use to index your fatigue (e.g., daily fingerboard routine runs, etc.)? These, and many more, are excellent ways to measure your training and overall health.
Make sure you don’t overtrain. This is a tough one, especially for endurance athletes. We all want to crush our goals. One of the easiest ways to prevent overtraining is to measure your training load. For this, you can use training applications or even a spreadsheet. Keeping track of how you feel after each workout can give you a signal when you’re overtraining. When increasing load, do it slowly and progressively, or have a coach direct your training. Make sure to recover, rest as needed, and seek expert guidance when you’re not sure you’re resting enough.
CONCLUSION
While HRV can be a useful tool for measuring the balance of the sympathetic and parasympathetic nervous systems, it is influenced by many factors and can be challenging to measure accurately.
There are many tools, indices, and procedures to index training state, recovery state, and overall health, but make sure you take care of the basics first, and the rest will fall into place.
REFERENCES
- Antelmi, I., Paula, R. S. D., Shinzato, A. R., Peres, C. A., Mansur, A. J., & Grupi, C. J. (2004). Influence of age, gender, body mass index, and functional capacity on heart rate variability in a cohort of subjects without heart disease. American Journal of Cardiology, 93(3), 381–385. https://doi.org/10.1016/j.amjcard.2003.09.065
- Balzarotti, S., Biassoni, F., Colombo, B., & Ciceri, M. R. (2017). Cardiac vagal control as a marker of emotion regulation in healthy adults: A review. Biological Psychology, 130, 54–66. https://doi.org/10.1016/j.biopsycho.2017.10.008
- Beauchaine, T. P., & Thayer, J. F. (2015). Heart rate variability as a transdiagnostic biomarker of psychopathology. International Journal of Psychophysiology: Official Journal of the International Organization of Psychophysiology, 98(2 Pt 2), 338–350. https://doi.org/10.1016/j.ijpsycho.2015.08.004
- Benjamim, C. J. R., Monteiro, L. R. L., Pontes, Y. M. de M., Silva, A. A. M. da, Souza, T. K. M. de, Valenti, V. E., Garner, D. M., & Cavalcante, T. C. F. (2021). Caffeine slows heart rate autonomic recovery following strength exercise in healthy subjects. Revista Portuguesa De Cardiologia, 40(6), 399–406. https://doi.org/10.1016/j.repce.2020.07.021
- Boudreau, P., Yeh, W. H., Dumont, G. A., & Boivin, D. B. (2012). A circadian rhythm in heart rate variability contributes to the increased cardiac sympathovagal response to awakening in the morning. Chronobiology International, 29(6), 757–768. https://doi.org/10.3109/07420528.2012.674592
- Brunoni, A. R., Kemp, A. H., Dantas, E. M., Goulart, A. C., Nunes, M. A., Boggio, P. S., Mill, J. G., Lotufo, P. A., Fregni, F., & Benseñor, I. M. (2013). Heart rate variability is a trait marker of major depressive disorder: Evidence from the sertraline vs. electric current therapy to treat depression clinical study. International Journal of Neuropsychopharmacology, 16(9), 1937–1949. https://doi.org/10.1017/S1461145713000497
- Campbell, B. I., Bove, D., Ward, P., Vargas, A., & Dolan, J. (2017). Quantification of Training Load and Training Response for Improving Athletic Performance. Strength & Conditioning Journal, 39(5), 3. https://doi.org/10.1519/SSC.0000000000000334
- Chalmers, J. A., Quintana, D. S., Abbott, M. J.-A., & Kemp, A. H. (2014). Anxiety Disorders are Associated with Reduced Heart Rate Variability: A Meta-Analysis. Frontiers in Psychiatry, 5, 80. https://doi.org/10.3389/fpsyt.2014.00080
- Deus, L. A., Sousa, C. V., Rosa, T. S., Filho, J. M. S., Santos, P. A., Barbosa, L. D., Silva Aguiar, S., Souza, L. H. R., & Simões, H. G. (2019). Heart rate variability in middle-aged sprint and endurance athletes. Physiology & Behavior, 205, 39–43. https://doi.org/10.1016/j.physbeh.2018.10.018
- Earnest, C. P., Blair, S. N., & Church, T. S. (2012). Heart rate variability and exercise in aging women. Journal of Women’s Health (2002), 21(3), 334–339. https://doi.org/10.1089/jwh.2011.2932
- Elgendi, M., Jonkman, M., & DeBoer, F. (2011). Heart Rate Variability and the Acceleration Plethysmogram Signals Measured at Rest. In A. Fred, J. Filipe, & H. Gamboa (Eds.), Biomedical Engineering Systems and Technologies (pp. 266–277). Springer. https://doi.org/10.1007/978-3-642-18472-7_21
- Fallen, E. L., Kamath, M. V., Tougas, G., & Upton, A. (2001). Afferent vagal modulation: Clinical studies of visceral sensory input. Autonomic Neuroscience: Basic and Clinical, 90(1), 35–40. https://doi.org/10.1016/S1566-0702(01)00265-X
- Gillie, B. L., & Thayer, J. F. (2014). Individual differences in resting heart rate variability and cognitive control in posttraumatic stress disorder. Frontiers in Psychology, 5, 758. https://doi.org/10.3389/fpsyg.2014.00758
- Gross, J. J. (2001). Emotion Regulation in Adulthood: Timing Is Everything. Current Directions in Psychological Science, 10(6), 214–219. https://doi.org/10.1111/1467-8721.00152
- Gross, J. J., & Thompson, R. A. (2007). Emotion Regulation: Conceptual Foundations. In Handbook of emotion regulation (pp. 3–24). The Guilford Press.
- Hill, L., & Siebenbrock, A. (2009). All are measures created equal? Heart rate variability and respiration. Biomed Sci Instrum, 45, 71-76. Biomedical Sciences Instrumentation, 45, 71–76.
- Hinde, K., White, G., & Armstrong, N. (2021). Wearable Devices Suitable for Monitoring Twenty Four Hour Heart Rate Variability in Military Populations. Sensors (Basel, Switzerland), 21(4), 1061. https://doi.org/10.3390/s21041061
- Laborde, S., Mosley, E., & Mertgen, A. (2018). Vagal Tank Theory: The Three Rs of Cardiac Vagal Control Functioning – Resting, Reactivity, and Recovery. Frontiers in Neuroscience, 12. https://www.frontiersin.org/articles/10.3389/fnins.2018.00458
- Martins-Pinge, M. C. (2011). Cardiovascular and autonomic modulation by the central nervous system after aerobic exercise training. Brazilian Journal of Medical and Biological Research, 44, 848–854. https://doi.org/10.1590/S0100-879X2011007500102
- Mather, M., & Thayer, J. (2018). How heart rate variability affects emotion regulation brain networks. Current Opinion in Behavioral Sciences, 19, 98–104. https://doi.org/10.1016/j.cobeha.2017.12.017
- Park, G., & Thayer, J. F. (2014). From the heart to the mind: Cardiac vagal tone modulates top-down and bottom-up visual perception and attention to emotional stimuli. Frontiers in Psychology, 5, 278. https://doi.org/10.3389/fpsyg.2014.00278
- Plews, D. J., Scott, B., Altini, M., Wood, M., Kilding, A. E., & Laursen, P. B. (2017). Comparison of Heart-Rate-Variability Recording With Smartphone Photoplethysmography, Polar H7 Chest Strap, and Electrocardiography. International Journal of Sports Physiology and Performance, 12(10), 1324–1328. https://doi.org/10.1123/ijspp.2016-0668
- Quintana, D. S., Alvares, G. A., & Heathers, J. a. J. (2016). Guidelines for Reporting Articles on Psychiatry and Heart rate variability (GRAPH): Recommendations to advance research communication. Translational Psychiatry, 6(5), Article 5. https://doi.org/10.1038/tp.2016.73
- Reichel, T., Hacker, S., Palmowski, J., Boßlau, T. K., Frech, T., Tirekoglou, P., Weyh, C., Bothur, E., Samel, S., Walscheid, R., & Krüger, K. (2022). Neurophysiological Markers for Monitoring Exercise and Recovery Cycles in Endurance Sports. Journal of Sports Science & Medicine, 21(3), 446–457. https://doi.org/10.52082/jssm.2022.446
- Shaffer, F., & Ginsberg, J. P. (2017). An Overview of Heart Rate Variability Metrics and Norms. Frontiers in Public Health, 5, 258. https://doi.org/10.3389/fpubh.2017.00258
- Shaffer, F., McCraty, R., & Zerr, C. L. (2014). A healthy heart is not a metronome: An integrative review of the heart’s anatomy and heart rate variability. Frontiers in Psychology, 5, 1040. https://doi.org/10.3389/fpsyg.2014.01040
- Silverthorn, D. U., Johnson, B. R., Ober, W. C., Garrison, C. W., & Silverthorn, A. C. (2013). Human physiology: An integrated approach (6th ed). Pearson Education.
- Souza, H. C. D., Philbois, S. V., Veiga, A. C., & Aguilar, B. A. (2021). Heart Rate Variability and Cardiovascular Fitness: What We Know so Far. Vascular Health and Risk Management, 17, 701–711. https://doi.org/10.2147/VHRM.S279322
- Stein, P. K., & Pu, Y. (2012). Heart rate variability, sleep and sleep disorders. Sleep Medicine Reviews, 16(1), 47–66. https://doi.org/10.1016/j.smrv.2011.02.005
- Stenfors, C. U. D., Hanson, L. M., Theorell, T., & Osika, W. S. (2016). Executive Cognitive Functioning and Cardiovascular Autonomic Regulation in a Population-Based Sample of Working Adults. Frontiers in Psychology, 7. https://www.frontiersin.org/articles/10.3389/fpsyg.2016.01536
- Strüven, A., Holzapfel, C., Stremmel, C., & Brunner, S. (2021). Obesity, Nutrition and Heart Rate Variability. International Journal of Molecular Sciences, 22(8), Article 8. https://doi.org/10.3390/ijms22084215
- Tarvainen, M. P., Lipponen, J., Niskanen, J.-P., & Ranta-aho, P. O. (n.d.). User guide – kubios. Kubios. Retrieved February 24, 2023. https://www.kubios.com/downloads/Kubios_HRV_Users_Guide.pdf
- Tegegne, B. S., Man, T., van Roon, A. M., Snieder, H., & Riese, H. (2020). Reference values of heart rate variability from 10-second resting electrocardiograms: The Lifelines Cohort Study. European Journal of Preventive Cardiology, 27(19), 2191–2194. https://doi.org/10.1177/2047487319872567
- Thamm, A., Freitag, N., Figueiredo, P., Doma, K., Rottensteiner, C., Bloch, W., & Schumann, M. (2019). Can Heart Rate Variability Determine Recovery Following Distinct Strength Loadings? A Randomized Cross-Over Trial. International Journal of Environmental Research and Public Health, 16(22), 4353. https://doi.org/10.3390/ijerph16224353
- Thayer, J. F., Hansen, A. L., Saus-Rose, E., & Johnsen, B. H. (2009). Heart rate variability, prefrontal neural function, and cognitive performance: The neurovisceral integration perspective on self-regulation, adaptation, and health. Annals of Behavioral Medicine: A Publication of the Society of Behavioral Medicine, 37(2), 141–153. https://doi.org/10.1007/s12160-009-9101-z
- Thayer, J. F., & Lane, R. D. (2000). A model of neurovisceral integration in emotion regulation and dysregulation. Journal of Affective Disorders, 61(3), 201–216. https://doi.org/10.1016/s0165-0327(00)00338-4
Heart Rate Variability
Table of Contents